Meet Tier 3 AMH Requirements
Our reporting helps you meet the requirements of the North Carolina Medical Home program, including:
Collecting, organizing, and making use of aggregated information on attributed beneficiaries
Periodically assessing and reporting on care management encounters and clinical performance
Identifying patient and population needs and actionable information to help close gaps and ensure compliance with AMH Tier 3 service-level agreements with PHPs
Your Dedicated Analytics Representative
Your rep works to understand your business analytics and reporting requirements, designs a tailored strategy, and helps implement that strategy to improve business decision-making.
Ad Hoc
Reporting
Solve problems to advance your unique business objectives with analytics based on your exact needs
-
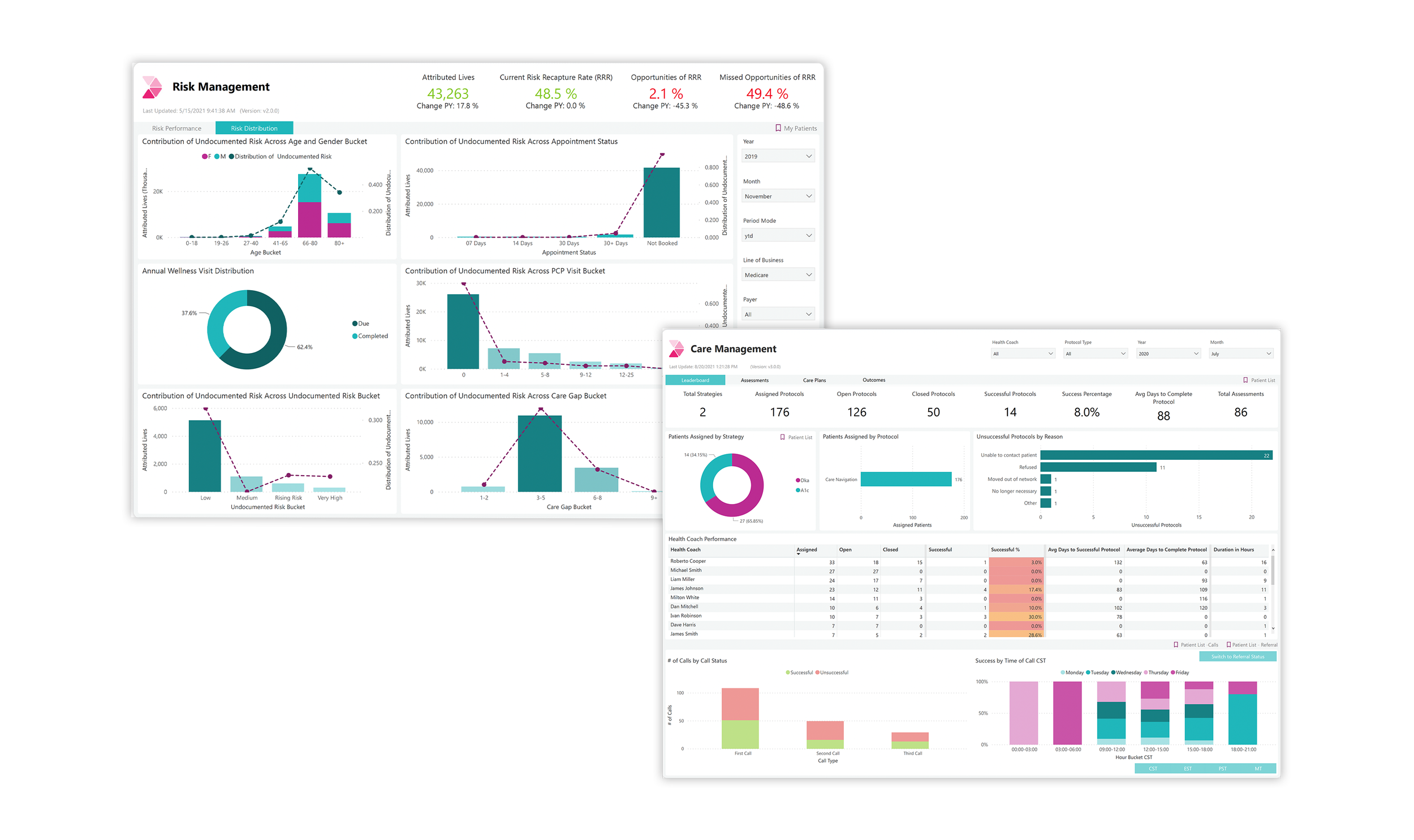
-Care Management Performance Dashboard
-Attribution Dashboard
-Risk Management Dashboard
-Quality Management Dashboard
-Utilization Dashboard
-PHP Risk List Reports
-
-Cost Dashboard
-Network Leakage Dashboard
InGraph Dashboards & Reports
Robust EmPACC platform includes:
7 Standard Dashboards
50 NQF & AHRQ KPIs (Key Performance Indicators)
10 NC Medicaid AMH Tier 3 Priority Quality Measures
11 Care Management Performance KPIs

Ready to Empower Your Practice?